Neuromodulation Therapies for Treatment-Resistant Depression

If you’ve been struggling with treatment-resistant depression, there’s new hope. Neuromodulation therapies, like the repetitive Transcranial Magnetic Stimulation (rTMS) program, offer a promising alternative. This program was launched by Waypoint Centre for Mental Health Care in partnership with Sunnybrook Health Sciences Centre.
This innovative approach to Neuromodulation for Treatment-Resistant Depression aims to provide specialized care closer to home. The rTMS program is recommended for individuals suffering from refractory depression. It has reported a 50% remission rate after six months of treatment.
With the capacity to serve 70 to 80 patients annually, this Brain Stimulation Therapies initiative is making a significant impact. It helps those who have not responded to traditional antidepressants or therapies.

By administering a full course of treatment five times a week for six weeks, the rTMS program provides a comprehensive and convenient approach to care. It serves both inpatients and outpatients at Waypoint. This program is accessible to those in need, addressing the challenges faced by one in five Canadians who experience a mental health or addiction concern.
Understanding Treatment-Resistant Depression and Its Impact on Mental Health
Neuropsychiatric disorders, like treatment-resistant depression, are big challenges for people and healthcare. In Canada, one in five people face mental health or addiction issues. This shows we really need new ways to treat depression.
Identifying Signs of Treatment Resistance
Treatment-resistant depression means not getting better with many tries of medicines and therapies. People with it often feel very sad, lose interest in things, and have trouble sleeping or eating. They also find it hard to do everyday tasks.
The Psychological and Social Impact
Living with treatment-resistant depression can really hurt your life, relationships, and happiness. People might feel hopeless, think poorly of themselves, and feel alone. These feelings make their mental health problems worse.
Current Treatment Challenges
For those with treatment-resistant depression, usual treatments like medicines and talk therapy don’t always work. Not having access to mental health services in some places and needing better treatments are big problems. These issues make it hard for people to find relief from their symptoms.
| Statistic | Value |
|---|---|
| rTMS program expected to treat | 70 to 80 people annually |
| Remission rate after six months using rTMS | 50% |
| Canadians experiencing mental health or addiction concerns | 1 in 5 |
Neuromodulation for Treatment-Resistant Depression: An Overview
People with treatment-resistant depression now have new hope. Neurostimulation Techniques and Brain Stimulation Therapies are changing mental health care. Treatments like repetitive transcranial magnetic stimulation (rTMS) use magnetic pulses to help brain cells.
These therapies are given in comfortable settings. They offer hope to those who haven’t found relief before. Studies show a 50% remission rate after six months with these treatments.
These treatments can help many people. A single machine can treat 70 to 80 people annually. This is important because one in five Canadians face mental health or addiction issues.
The treatment involves five sessions per week for six weeks. Each session is about five minutes. This approach has even led to the swift discharge of some patients.
| Key Statistic | Value |
|---|---|
| Remission rate after six months | 50% |
| Annual treatment capacity per machine | 70-80 people |
| Cost of machine | $180,000 |
| Canadians experiencing mental health or addiction concerns | 1 in 5 |
| Treatment sessions per week | 5 |
| Duration of treatment | 6 weeks |
| Duration of each session | 5 minutes |
Healthcare providers are using Neurostimulation Techniques and Brain Stimulation Therapies to help those with treatment-resistant depression. These methods are changing how we treat mental health. They offer a new hope for those who haven’t found relief before.
 What recent research has revolutionized the field of neuroscience?
What recent research has revolutionized the field of neuroscience?
The Science Behind Brain Stimulation Therapies
Brain stimulation therapies for treatment-resistant depression focus on specific brain areas linked to mood. They aim to change brain activity in these areas. This helps the brain adapt and form new connections, leading to better mood over time.
Neural Pathways and Depression
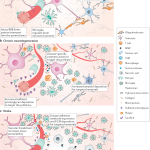
Studies have shown that certain brain circuits are key in depression. The prefrontal cortex, limbic system, and monoaminergic systems are involved. These areas control mood, emotions, and reward processing, but are often out of balance in people with Neuropsychiatric Disorders.
Mechanism of Action in Neuromodulation
Therapies like transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS) directly affect these pathways. They use electrical or magnetic stimulation to help balance brain function. This is crucial for treating Neuromodulation for Treatment-Resistant Depression.
Neuroplasticity and Recovery
The brain’s ability to change and form new connections is key. Brain stimulation therapies take advantage of this. By targeting specific areas, they can lead to lasting changes in brain activity. This improves mood and helps fight off depression.
| Therapy | Mechanism of Action | Effectiveness |
|---|---|---|
| Transcranial Magnetic Stimulation (TMS) | Applies targeted magnetic pulses to stimulate specific brain regions | 44.9% of participants in the active treatment arm demonstrated a remission rate compared to 21.8% in the control group. |
| Transcranial Direct Current Stimulation (tDCS) | Applies a weak direct current to the scalp to modulate brain activity | The study included 174 adult participants with a diagnosis of severe to moderate depression, and participants had a 10-week course of treatment with five 30-minute sessions a week for the first three weeks followed by three 30-minute sessions a week for the next seven weeks. |
Transcranial Magnetic Stimulation (TMS): A Revolutionary Approach
Transcranial Magnetic Stimulation (TMS) is a new way to treat depression that doesn’t involve surgery. It uses magnetic pulses to wake up parts of the brain. This helps control mood.
Unlike pills, TMS is done in short, painless sessions. People usually go five times a week for six weeks. Each session is just five minutes, and you can go back to your day right after.
Studies show TMS can help 50% of people with depression feel better after six months. It’s also being tested for other issues like OCD and quitting smoking.
| Neuromodulation Technique | Invasiveness | Depth of Penetration | Precision |
|---|---|---|---|
| Transcranial Magnetic Stimulation (TMS) | Non-invasive | Limited to cortical regions | Relatively focal |
| Deep Brain Stimulation (DBS) | Invasive | Reaches deep brain structures | Highly targeted |
| Vagus Nerve Stimulation | Invasive | Targets subcortical structures | Relatively broad |
| Electroconvulsive Therapy (ECT) | Invasive | Widespread brain modulation | Broad and non-selective |
As scientists keep studying TMS and other brain treatments, we’re on the verge of big changes. These could lead to better care for mental health. It’s a step towards more tailored and effective treatments.
Deep Brain Stimulation: Advanced Treatment for Severe Cases
For those with treatment-resistant depression, Deep Brain Stimulation (DBS) is a new hope. It’s a surgery that implants electrodes in the brain. These electrodes send electrical impulses to help manage depression symptoms.
Surgical Procedure and Implementation
The DBS surgery is done under general anesthesia. Thin wires with electrodes are placed in the brain’s mood centers. Then, a small device like a pacemaker is put under the skin. This device sends electrical impulses to the brain, helping to ease depression.
Target Brain Areas and Effectiveness
DBS targets specific brain areas for depression treatment. Studies show it works well, with some patients seeing big mood improvements. For example, a Nature Medicine study found 44.9% of DBS patients got better, compared to 21.8% without it.
Recovery and Monitoring Process
Recovering from DBS surgery takes weeks to months. Doctors watch how the brain responds and adjust the settings as needed. Regular check-ups ensure the treatment is working right.
Deep Brain Stimulation is a big step forward for severe depression treatment. It targets brain areas and changes how they work. This new method gives hope to those who haven’t found relief with other treatments. As technology advances, DBS could bring lasting relief and better lives for many.
Vagus Nerve Stimulation: A Long-term Treatment Option
Vagus Nerve Stimulation (VNS) is a promising long-term treatment for those with treatment-resistant depression. It uses neuromodulation to stimulate the vagus nerve. This helps control brain activity linked to mood.
 Neuropharmacology: Targeted Drug Delivery for Neurological Disorders
Neuropharmacology: Targeted Drug Delivery for Neurological Disorders
The vagus nerve plays a key role in the parasympathetic nervous system. It helps manage heart rate, digestion, and emotions. VNS aims to balance the sympathetic and parasympathetic systems in those with treatment-resistant depression.
VNS offers a continuous treatment that can be adjusted as needed. The device, implanted under the skin, sends electrical impulses to the vagus nerve. This helps modulate brain activity and reduce depressive symptoms.
| Key Benefits of Vagus Nerve Stimulation | Considerations |
|---|---|
|
|
It’s crucial to discuss Vagus Nerve Stimulation with a healthcare provider. They can help decide if it’s right for you. Understanding its benefits and considerations can help those with treatment-resistant depression. It’s a step towards managing their mental health.
Electroconvulsive Therapy in Modern Practice
Electroconvulsive Therapy (ECT) has changed a lot in recent years. It’s now seen as a safe and effective treatment. At Waypoint Centre for Mental Health Care, Dr. Plabon Ismail oversees ECT. He makes sure patients are safe and get the most from the treatment.
Modern ECT Techniques
Today’s ECT is much better for patients. General anesthesia and muscle relaxants make the process comfortable and safe. New ways of placing electrodes and adjusting electrical settings have also reduced side effects. This makes ECT a good choice for those looking for Depression Treatment Innovations.
Safety Protocols and Patient Care
At Waypoint, the Electroconvulsive Therapy process is carefully watched to ensure safety and care. Before treatment, patients get full medical checks. During the treatment, their vital signs are closely monitored. Afterward, they are watched closely to make sure they are okay.
The results show that Electroconvulsive Therapy works well for people with treatment-resistant depression (TRD). After the initial treatment, patients see a 29.4% improvement on the HRSD-24. The response rate is 25.2%. After tapering, the remission rate is 34.8%, and during the prevention phase, the improvement is 60.1%. These numbers show how effective Electroconvulsive Therapy is as a Depression Treatment Innovation for TRD.
| Metric | Value |
|---|---|
| Remission rate after the acute phase | 16.1% |
| Mean reduction from baseline on the HRSD-24 after the acute phase | 29.4% |
| Response rate after the acute phase | 25.2% |
| Mean reduction from baseline after the tapering phase | 42.6% |
| Response rate after the tapering phase | 49.6% |
| Remission rate after the tapering phase | 34.8% |
| Mean reduction from baseline during the symptom-based relapse prevention phase | 60.1% |
| Patients who completed eligibility for the relapse prevention phase | 43 out of 61 |
| Patients who relapsed during the relapse prevention phase | 7 out of 43 |
Innovative Neurostimulation Techniques and Future Developments
The field of Neurostimulation Techniques is growing fast. New technologies and therapies are coming out to help with treatment-resistant depression. Researchers and clinicians are looking into new ways to make treatments better, safer, and more effective.
One new thing is the use of special TMS helmets. These helmets use advanced coils for a more focused treatment. This makes TMS useful for more than just depression. Teams like Waypoint and Sunnybrook are working together to make these advancements.
Ultrasound neuromodulation is another area to watch. Transcranial focused ultrasound (tFUS) can target deep brain areas without being too invasive. It works by affecting cells in a new way. Studies show it can make brain activity better or worse, with few side effects.
| Neurostimulation Technique | Key Features | Potential Applications |
|---|---|---|
| Transcranial Magnetic Stimulation (TMS) Helmets |
|
|
| Transcranial Focused Ultrasound (tFUS) |
|
|
As Neurostimulation Techniques keep getting better, we’ll see even more new ideas. These advancements could lead to treatments that are more effective, tailored to each person, and easier to get. This is exciting for those who need help with treatment-resistant depression and beyond.
Patient Selection and Treatment Planning
Choosing the right patients for neuromodulation therapies is key to treating depression effectively. At Waypoint, the rTMS program only accepts patients through referrals. General practitioners check if the treatment is right for their patients. This careful step helps find those who will benefit most from these new treatments.
Assessment Criteria
Mental health experts at Waypoint use a detailed assessment to see if a patient is a good fit for these therapies. They look at how severe the depression is, the patient’s treatment history, and their overall mental health. This ensures that Neuromodulation for Treatment-Resistant Depression is the best choice.
By considering each patient’s unique needs and medical history, the team creates a treatment plan that works best. This approach helps increase the chances of a successful outcome.
 The Role of Neuroinflammation in Neurodegenerative Diseases
The Role of Neuroinflammation in Neurodegenerative Diseases
Customizing Treatment Protocols
At Waypoint, treatment plans for neuromodulation therapies are made just for each patient. Their $180,000 rTMS machine can help 70 to 80 people a year. The team works hard to create a plan that tackles the specific challenges of treatment-resistant depression.
By using the latest in Neuromodulation for Treatment-Resistant Depression, Waypoint aims to help patients. They support their journey towards better mental health and well-being.






